Beta cells 101: Explaining the role of beta cells in type 1 diabetes with Professor Beta T1D
Posted: June 30, 2025 | Word Count: 634

Sponsored by Sanofi
It's an unfortunate reality that myths and misconceptions about type 1 diabetes (T1D) are widespread today, leading to significant awareness gaps that ultimately make it harder for people to understand their own risk of developing the disease. Consider this: While many believe that T1D is a juvenile disease, it can impact anyone at any age. Others think it begins only when symptoms appear, when in fact, the disease progresses gradually in stages over time.
These misconceptions extend to a root cause of the disease. T1D is not simply caused by a lack of insulin; it's a result of the autoimmune response in which the body mistakenly attacks its own healthy beta cells. The destruction of beta cells is central to the development of Stage 3 T1D, which is why understanding beta-cell function is foundational to understanding the progression of T1D. Below, explore why beta cells are such a critical piece of the T1D progression puzzle.
The role of beta cells
Located in the pancreas, beta cells are responsible for insulin production, insulin storage, and the regulated release of insulin. Beta cells work to create glucose homeostasis (i.e., keeping blood glucose levels within a healthy range) and precisely respond to changes in the body's metabolic status due to food intake and other factors. In T1D, an autoimmune-mediated response – likely initiated by a complex interplay of genetic susceptibility and environmental triggers – targets and destroys these insulin-producing beta cells.
Ongoing, underlying beta-cell destruction is a critical marker of progressive autoimmune T1D. This progression is what defines the stages of T1D. Beta cell destruction can begin as early as four to six years before clinical symptoms appear. In Stage 2 T1D, more damaged beta cells release autoantigens which causes T1D autoantibodies to develop in the blood in response to the autoimmune attack. T1D screening through a blood test can detect these autoantibodies early, potentially identifying T1D in its early stages – before symptoms even emerge.
As we continue to learn more about the unique role of beta cells in T1D, education around beta-cell function becomes critical. That's where "Professor Beta T1D" comes in.
Meet Professor Beta T1D
To help demystify the science behind T1D and build a better understanding of beta-cell function, Sanofi created Professor Beta T1D – an animated, educational digital avatar dedicated to making beta-cell science more accessible and digestible. Professor Beta T1D's goal is to highlight the unique impact of beta cells in T1D.
Professor Beta T1D is bringing his expertise to HCPs through social channels like X, Instagram, and LinkedIn. Professor Beta T1D is a healthy beta cell living his best life, seeking to keep calm and carry on in the face of T1D.
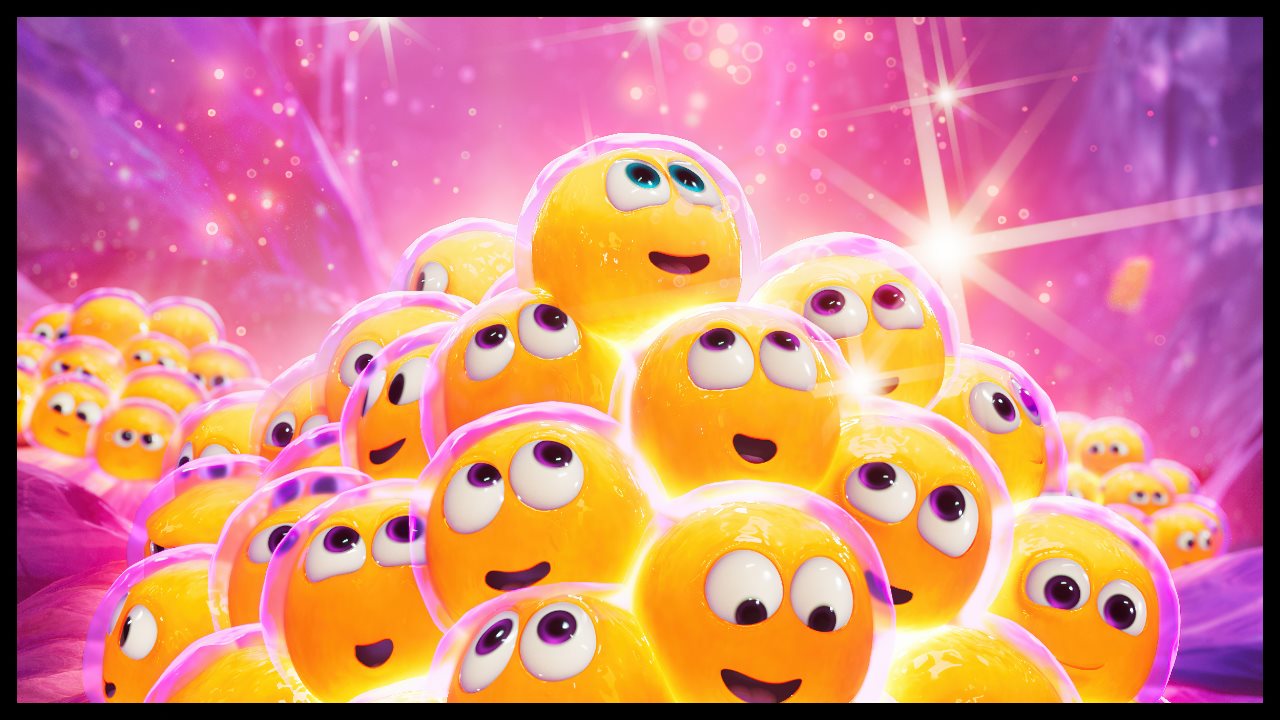
As an ambassador for the clusters of other beta cells, Professor Beta T1D is highly knowledgeable, but also frustrated, fighting to be heard before it's too late. As a strong believer that there's a "beta way to look at T1D," there are two things Professor Beta T1D wants others to know about beta-cell function:
- Beta-cell function determines disease progression and an individual's T1D journey. As measured by C-peptide, beta-cell function can indicate patients' level of remaining beta-cell activity and help determine the extent of autoimmune T1D progression.
- Beta cells define clinical outcomes, because some functional beta cells are better than none! It has been observed that in T1D even low beta cell function can produce adequate endogenous insulin to maintain glycemic control.
Insights into how beta cells influence T1D are key to understanding disease progression and may help inform the development of novel disease management approaches. Learn more about beta-cell function on www.betawayt1d.com.
Sanofi does not provide medical advice, diagnosis, or treatment – information is provided for educational purposes only. Patients are directed to their doctor if they have any questions about their health or disease management.
Includes Multiple Photos


